This biography is based on secondary source material listed in the bibliography. Much of the information in these sources comes from various interviews with Emily Siedeberg-McKinnon’s niece, Emily Host.
1896 GRADUATE

Contents
High Expectations From a Young Age
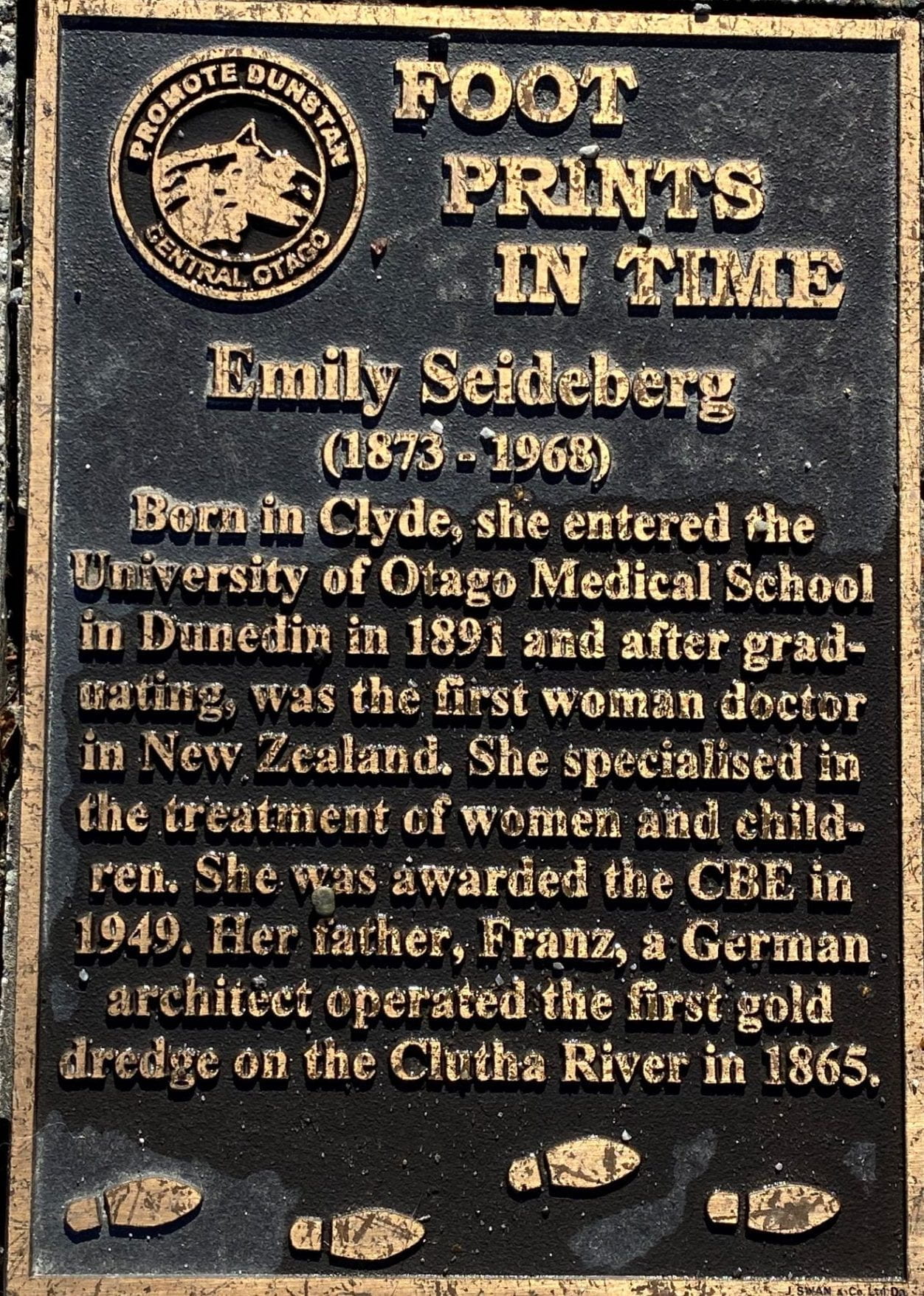
Emily Hancock Siedeberg was born on 17 February 1873 to Anna Thompson and Franz David Siedeberg.[1] Emily was their third child out of four children. Franz was a German Jewish architect from Memel, Prussia (now Klaipėda, Lithuania).[2] He migrated to New Zealand in 1861 in the hopes of finding success in the gold mining industry.[3] Anna Thompson was a Northern Irish Quaker and the daughter of George Thompson, a successful barrister and solicitor from Trinity College, Dublin.[4] Franz and Anna married in 1867 in St Paul’s Church, Dunedin.[5] The couple settled in Clyde, the mining centre of the Clutha River valley in the South Island.[6] When Emily was three years old, the family moved to York Place in Dunedin, where Franz became a successful builder.[7] Emily remembered having a “happy childhood with never a cross word between her parents”.[8]
From a young age, Franz had high expectations for his daughter. His opinion on education was relatively progressive compared to many of his contemporaries, suggesting that Emily might like to become a doctor when she was only ten years old.[9] At this time, medicine was not considered a profession for women.[10] She overheard her parents in discussion: “I think we will make a doctor of Emily”.[11] While her first reaction was, “Only men are doctors”, she later came to the conclusion that “it would be a grand life to drive about all day in a carriage”.[12] Franz later bought her the book ‘Our Famous Women’, which covered the struggles of the Blackwell sisters and other progressive women to “win a place in the world… To Emily this book opened up vistas of what life meant, the struggles ahead, the difficulties to overcome. She had been shown a purpose in life and so grew up with the sure knowledge that it was her destiny to be a doctor”.[13]
Emily attended the Normal School located on Moray Place and achieved academically well, so much so that she received a board scholarship to attend Otago Girls’ High School.[14] She attended Otago Girls’ until age 17 when she began the process of enrolling in the Otago Medical School.[15] This process was relatively gruelling, and no one had yet been successful. A Miss Tracy had attempted to enrol in the Otago Medical School a few years prior but failed to win the support of the staff.[16] One medical man remarked: “Why should a woman unsex herself by giving way to a morbid craving which, from its popularity, can only be likened to an epidemic of insanity … It is presumed that the candidate… is unaware of what she will have to go through, and she must assuredly give in after a short time, feeling herself degraded”.[17]
Isolation at University and Overcoming her Fears
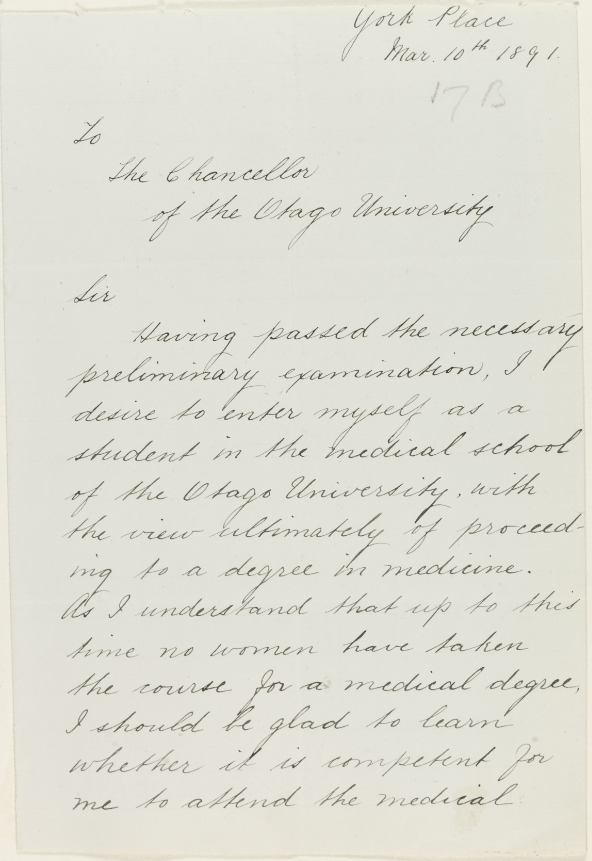
On 10 March 1891, Emily Siedeberg wrote a letter to the Chancellor of the University of Otago, expressing her desire to enrol in the medical school.[18] The University staff voted in favour of her on the basis that the University of Otago Council had announced the Medical School would be open to both men and women when it was established in 1885.[19] Despite this, two staff members believed women should be kept separate, and the other seven thought they should be treated the same and were willing to teach mixed classes.[20] Concurrently to her admission to the University, Emily wrote to the trustees of Dunedin Hospital to enquire if she could attend the hospital as a medical student. The trustees approached the nine staff of the hospital, six of whom voted against Emily’s attendance. Two of the staff were in favour, and the final member recommended that she attend a medical school in Great Britain that had been established specifically for the purpose of training women doctors.[21] However, upon further discussion, they determined that if the University was willing to accept her, they could not reject her request for admission to the hospital.[22] Thus, on 29 April 1891, Emily Hancock Siedeberg was added to the register of medical students at the University of Otago.[23] In comparison to other countries, Emily’s entrance was relatively smooth and faced little controversy in the media – especially because most universities in Great Britain were allowing women to attend classes but were refusing to grant degrees, something that Emily did not have to deal with.[24]
Despite the joy that came with her acceptance to the medical school, Emily felt a lot of pressure to be successful; she believed that she was setting an example for future women to study medicine in New Zealand.[25] The Dean, Dr Scott, had also been quite upfront with her about how she would need to conduct herself in order to be accepted by the men in her classes: “He led me to understand that the attitude of the students towards me would depend entirely on how I conducted myself. The good old Victorian mothers had trained their daughters in self-respect- ‘keep men at a distance, don’t allow them to touch you or take liberties, never show your feelings of look invitingly at them.’ So I behaved accordingly and no frivolities or incidents of much importance occurred in the dissecting room or elsewhere”.[26] He advised that if she could hold her own in a class with students who were prone to doing pranks, then she would be just fine.[27] Her mother also had advised her to “to keep men at a distance and never to show her feelings”.[28] These two pieces of advice left her relatively isolated in her first year, so she was delighted when her friend from Otago Girls’ High, Margaret Cruickshank, entered medical school the following year.[29]
Unfortunately, the Dean was correct; the men in the class were not delighted to see her: “fearing embarrassment and also a little concerned lest she receive special treatment … they [the male students] indoctrinated her very swiftly, making no effort to moderate their language, trying vainly to upset her, watching constantly to see if she flinched. She did not”.[30] This was all put to the test the first time she was in the theatre and she witnessed her first flow of blood. “I knew the eyes of students, doctors and nurses were on me. Pride and determination took me in their grip. Just as the knife went in and I knew blood would flow, I turned my eyes to the floor and kept them there. I saw not a drop of blood. I emerged victorious, and after that it was easier”.[31] Contrary to many of the mythical stories that arose after her graduation, the rest of her studies continued relatively smoothly. One such story argued that the male students pelted her with human flesh in the dissecting rooms and that she faced constant persecution. When recalling it many years later, Emily said that there was only “‘one trifling occasion when a few pieces from another dissecting table came in my direction’, but on the whole her fellow students were ‘quite well-behaved young men’“.[32]
One notable moment from Emily’s time at University was in her third year when, at age 20, she signed the petition in support of women’s suffrage along with her mother and older sister.[33] Emily completed her studies after her fifth year in 1895 and graduated in 1896 with an M.B Ch.B, making her the first woman doctor graduate in New Zealand.[34] This was completed in one year less than was usual as she had been permitted to complete two years’ work in one so that she could attend a special conference in Edinburgh.[35] Before leaving for Edinburgh, however, she completed a short locum for Dr Truby King at Seacliff Lunatic Asylum.[36]
Further Studies, Establishing Her Practice & Specialising in Women’s Health
While on her locum at Seacliff, she met Dr Lindo Ferguson, who suggested that she undertake postgraduate studies at the Rotunda Hospital in Dublin.[37] Emily agreed and moved to Dublin, where she enrolled to study obstetrics.[38] She then moved on to Berlin to complete postgraduate courses in gynaecology and children’s and skin diseases.[39] As with most women doctors at this time, she specialised in areas “within the conventional stereotypes of women’s strengths”.[40] This was common for the period, with the first women to practice in New Zealand specialising in areas relating to these stereotypes: Kathleen Todd in child psychology; Agnes Bennett, Doris Gordon, and Emily Siedeberg in obstetrics; and Muriel Bell in nutrition.[41] Before setting off for Berlin, Emily wondered what the attitude towards woman doctors would be in Germany. She found it to be progressive compared to other areas she had visited. Many of the men were sympathetic, and the well-known Professor Lassar had even written a pamphlet encouraging women to take up medicine as a career.[42]

Emily returned to Dunedin at the end of 1897, where she set up her own private practice with financial aid from her father.[43] Her sister moved in with her to become the clinic’s housekeeper and organise all of their social events.[44] Emily maintained this practice for thirty years.[45] She was the only woman practitioner in Dunedin for the first twenty of these, meaning that competition was minimal.[46] Business was initially slow, but she was able to continue due to the aid from her father, who gave her the house at York Place with consulting and waiting rooms and a horse and gig.[47] Her first patients were women and children, and she slowly built up her client list with her reputation of never saying no when someone was in need of help, no matter the conditions: “day or night, hail, snow or storm, in good health or off-colour”.[48]
When needed, Emily ordered a trap from the stables to help her travel; she did not buy one as she was not yet busy enough to warrant it.[49] She recalled one night when a patient from outside the city called for help: “She walked to the stables and knocked loudly on the door. There was no answer. Dr Siedeberg remembered the policeman’s whistle she carried as a precaution in her handbag. From the middle of the street she blew it and almost at once a burly policeman came running along. The authoritarian voice of the law, “Open in the name of the King!”, soon brought the driver to the door”.[50]
Within the first few years of her practice, Emily also undertook further study at the University of Otago and was awarded a Bachelor of Science degree in 1901.[51] In 1900, she was appointed as the Honorary Medical Officer with the Society for the Protection of Women and Children.[52] In 1905 she was appointed as the first medical officer (and later superintendent) of St. Helen’s Maternity Hospital in Dunedin, which she received through the influence of one of her patients from her private clinic, Harriet Morison.[53] This hospital was established by the Prime Minister of New Zealand (Mr R. J. Seddon) for the training of midwives and to provide maternity care to low-income women.[54] She held this part-time position from when the hospital opened in 1905 to when it closed in 1938 to give way to Queen Mary Hospital.[55]
Further appointments, World Wars One and Two, & Establishing the First Antenatal Clinic
In 1907, Emily was appointed at the medical office for the Caversham Receiving Home, which she held until 1930.[56] She took a break from her New Zealand work in 1912 to travel to the University of Edinburgh for further postgraduate studies.[57] In 1915, she applied to the “Scottish Women’s Hospital for Foreign Service” to go to Serbia or France to aid in the war effort but was advised that there were no vacancies in France and the Germans had broken through to Serbia already.[58] Instead, she was appointed as a house surgeon in the infirmary at Sheffield.[59] She returned to New Zealand in 1916 and an article in the Auckland Star from 16 May stated that the Royal Army Medical Corps was “not using the services of women doctors in any way”, quoting Emily: “there are still plenty of opportunities for New Zealand male doctors who come to England to offer their services”.[60] Indeed, Emily did not have much success in either war effort; in the Second World War she was given authority to run one of the “emergency precaution stations when there was a danger of Japanese invasion, which fortunately did not take place”.[61] However, despite her aid, her integrity was called into question when her loyalty to New Zealand was publicly questioned due to her German heritage. The Otago Daily Times soon received an emotional letter to the editor that sought to “quash any war time rumours concerning her German heritage and turn the focus back onto the motivations of the accusers”.[62] Notably, it also contained a remark that the monarchy also had German heritage.
Upon her return to New Zealand following World War One and her return to St Helen’s, Emily recognised the need for antenatal care in New Zealand. Thus, in 1918, Emily established the first antenatal clinic in New Zealand at St Helen’s Hospital.[63] This catalysed the development of antenatal clinics connected to all midwifery training schools around New Zealand.[64] Emily became renowned for her midwifery work. In 1920, “she recorded proudly that she had not a case of eclampsia (toxaemia) for 11 years, at a time when this disease was a major killer of women in childbirth”.[65]
In 1921, Emily took up a ten-year position as an anaesthetist at the Dental School at the University of Otago, which she held concurrent to her position at St Helen’s.[66] An issue arose in 1922 when a dental patient died under chloroform. In her testimony, she explained that, in her medical opinion, the conditions of the school were not at a high enough standard to promote patient safety.[67] Throughout this time, Emily also worked as a medical officer at the Caversham Industrial School (later the Girls’ Receiving Home), which was a reformatory institution located at Faversham, ran classes on nursing for the St John’s Ambulance Association, and was the surgeon for Rebekah Lodge, which had been established to aid women in need.[68]
Aiding “Fallen” Women
Emily’s interest in women’s health extended far beyond her work in antenatal clinics and her clinic. An incident in 1906 caused her to take a deep interest in “fallen women”; an interest that shocked her family and colleagues.[69] In 1906, Emily was called in to attend to a 25-year old single woman. She followed procedure and administered chloroform then carried out the examination. She found the woman had “extensive inflammation”, which the doctor she was working with, Dr Church, believed to be due to a “botched, illegal abortion”.[70] Emily applied the required antiseptic measures but though the woman appeared to improve, she died two days later. She recalled that a married man who had three children called into the nursing home, stating that he would pay all of the expenses. Emily was called to testify and ended up being “sternly reprimanded by the Chief Detective for not bringing the incident to the attention of the police as soon as the cause of the patient’s distress was known”.[71]
Though Emily was violently against prostitution, she took it upon herself to help prostitutes and women in need.[72] She brought these women into her home and tended to them, delivering and helping to find a suitable home for the babies. When her male colleagues heard about what she was doing, they condemned her. They believed that she was disgracing the medical profession by helping these “loose” women.[73]
Becoming the Spokesperson for Women’s Needs & Involvement in Organisations

Her work on women’s health extended beyond her interest in fallen women, as much of her activism centred upon welfare for women and children, “the rights which had been denied them in every direction through man-made laws”.[74] She argued that the Contagious Diseases Act should be “wiped off the statute book” because it was “an insult to womanhood”. It was repealed in 1910.[75] She also actively spoke in favour of women’s rights in regards to marriage. She argued that there should be strong measures in place to control venereal diseases, and that these diseases should be a legitimate reason for divorce.[76] Likewise, she appealed to the 1937 Committee of Inquiry at St Helen’s Hospital against hospital births being a requirement on the grounds that “a fair number of mothers are afraid of the infidelity of their husbands. That is a definite difficulty in persuading a woman to go into hospital, and even when they do go to hospital they are always anxious to get home again on that account”.[77]
Emily spoke out on the appointment of women on the police force and in the hospital and foster home inspection teams, equal opportunities for women in further education and employment, and the training of girls in domestic science.[78] She was also an avid supporter of the eugenic movement, as she believed that while the environment was important to the human race, it was less so than heredity.[79] In 1912, she reported to the First International Eugenics Congress in London, commenting that the Congress should “have the effect of placing Eugenics upon a scientific basis, and removing that frivolous idea of it which permeates the press in which eugenists are represented as forcibly mating two individuals who have nothing in common but good health, and no affection or respect for one another, the one thing which alone raises the mating of human beings above that of brute creation”.[80]
One of the reasons that her voice was so prominent in women’s rights activism was because of the various roles she held in New Zealand organisations, which she joined to fight “the wrongs of womankind as she would fight for the life of a patient”.[81] In 1899, she was instrumental in founding the Society for the Protection of Women and Children which sought to help women and children who were in abusive relationships.[82] She founded this society with the first woman law graduate from the University Otago, Ethel Benjamin. Emily was an Honorary Medical Officer and became an Honorary Life President in 1949.[83] In 1916, she helped to establish the Dunedin branch of the National Council of Women and was selected to be the representative of this council to welcome Jean Batten to New Zealand following her solo flight from London.[84] In 1921, she founded the New Zealand Medical Women’s Association and was elected as the first president.[85] The purpose of this association was to promote the interests of medical women and, where needed, act on their behalf.[86] She was also a founding member of the New Zealand Federation of University Women and the president of the Dunedin branch of the Plunket Society from 1933 to 1948.[87] In 1941, she achieved her dream of raising enough funds to open a community centre that would hold women’s events and meetings.[88] This dream came about from her trip to the first Women’s Conference at Honolulu in 1928, where she learnt about the Vancouver Women’s Building, which was established for a similar purpose.[89]
Arguably, the most significant impact she made, however, was in her efforts to expose legal injustices against women. As the president of the Society for the Protection of Women and Children, she succeeded in bringing forward concerns for women and succeeding in getting them placed in the statute book. For example, she spoke out for the raising of the legal age of consent for marriage from 12 to 16 years of age for girls and from 14 to 18 years of age for boys. She also argued for efforts to help the family man and protection for the wives: a husband should not be allowed to leave the country without written permission from their wife; a benefit should be given to a man that was not carelessly spending his money but could not earn enough to provide adequate clothing and food for his family; the mother and father would have equal rights over their children so that the mother could appoint a guardian should the father become invalid or a drunk; and that moral standards should be legitimate grounds for divorce for both the husband and wife.[90]
Because of her service, she was awarded the King’s Jubilee Medal in 1935 and the CBE in the King’s List of New Zealand Honours in 1949.[91] She was also awarded a life membership to the New Zealand branch of the British Medical Association in 1929 and a life membership to the New Zealand Registered Nurses’ Association in 1939.[92]
Driving, Finding her Home & Marrying Late
Emily was the second woman to drive and own a car in Dunedin. She had first seen an early motorcar in 1912 when she was in Edinburgh completing her postgraduate studies. She was a competent driver and drove well into her eighties. She recalled one incident when she was prosecuted for driving too fast. She had been driving faster than a walking pace (the “furious and dangerous speed” of only 15 miles per hour), however, she successfully defended herself and was not charged.[93]
Her family was also very important to her and she made sure to look after them as much as she could. Shortly after her father suddenly passed away in September 1902, she commissioned the architect James Louis Salmond to build a new house in front of the old family one in York Street. The new addition was large enough to house her mother, sister, and younger brother. Her younger brother lived there until his marriage in 1911 when he moved into the old family home next door. Her mother resided there for twenty years until her death in 1923 and her sister, a successful artist, stayed with Emily until she moved to Auckland in the 1920s.[94]

Emily’s niece, Emily Host, recalled that her aunt was quite conservative and held quite strongly to her Victorian beliefs. She advocated for domestic training for girls so as to prepare them for marriage, and she entered medical school with the hopes of finding a suitable husband at the medical school so that they could run a practice and raise children together.[95] Her plan, however, did not come to pass until much later. At age 55, she met a retired banker, James Alexander McKinnon, and married him on 8 October 1928 in Los Angeles, much to her family’s dismay who did not like him.[96] She started practising as Dr Siedeberg-McKinnon and the couple moved into a newly built house in Cairnhill Street in 1929. In 1938, Emily retired from active practice and the couple moved to a house in Cargill Street so that James was closer to the bowling green.[97]
James passed away in 1949 and Emily returned to her old home in York Street.[98] In 1951, she took her first trip on a plane to visit Emily in Africa and go on a safari with Joy Adamson (the author of Born Free).[99] In 1967, the Otago Girls’ High School named their new science wing the Emily Siedeberg Block and invited her to the ceremony, which was opened by Her Excellency Lady Fergusson.[100]
Death & Legacy
 As Emily’s health started to fade in the 1960s, she moved into the Presbyterian Social Service Association Home in Oamaru, where she passed away on 13 June 1968 at 95 years of age.[101] Emily’s decision to aid those in her community continued after her death. The primary beneficiaries of her will were her family, with the rest of it going to various organisations she had supported.[102] To honour her memory, Emily’s niece and her husband established the University of Otago Emily Siedeberg Scholarship in 2007 for female medical students. The award was worth NZ $1,250.[103]
As Emily’s health started to fade in the 1960s, she moved into the Presbyterian Social Service Association Home in Oamaru, where she passed away on 13 June 1968 at 95 years of age.[101] Emily’s decision to aid those in her community continued after her death. The primary beneficiaries of her will were her family, with the rest of it going to various organisations she had supported.[102] To honour her memory, Emily’s niece and her husband established the University of Otago Emily Siedeberg Scholarship in 2007 for female medical students. The award was worth NZ $1,250.[103]
“Emily Siedeberg was a woman of strength and determination, who rarely gave up once she had set her mind on something. Courageous and dignified, she proved herself a model woman doctor for the period by using her professional skills in the traditional female sphere of community service”.[104]
“She was not only the object of much curiosity and some resentment but a trendsetter”.[105]
In July 2023, Emily Siedeberg-McKinnon’s home and workplace received “the highest form of heritage recognition”. It was listed as a Category 1 Historic Place. Further information about the process can be viewed here: https://www.heritage.org.nz/news/stories/heritage-listing-for-health-trailblazer-s-house-and-surgery
Bibliography
Belgrave, Michael. 1988. “A Subtle Containment: Women in New Zealand Medicine, 1893-1941.” New Zealand Journal of History 22, no. 1 (April): 44-55.
Brookes, Barbara. 2017. “Emily Siedeberg, New Zealand’s first woman doctor.” Corpus. https://corpus.nz/emily-siedeberg-new-zealands-first-woman-doctor/.
Bryder, Linda. 2014. The Rise and Fall of National Women’s Hospital : A History. Auckland, New Zealand: Auckland University Press.
Creese, Mary R., and Thomas M. Creese. 2010. Ladies in the laboratory III: South African, Australian, New Zealand, and Canadian women in science : nineteenth and early twentieth centuries : a survey of their contributions. Lanham, Maryland: Scarecrow Press.
Cronin, Monica. 2018. “The Rare Privilege of Medicine: Women Anaesthetists in Australia and New Zealand.” ANZCA Bulletin 27, no. 1 (March): 8-9.
Cronin, Monica. 2017. “The Great Women of Anaesthesia: Emily Hancock Siedeberg McKinnon.” Geoffrey Kaye Museum of the Australian and New Zealand College of Anaesthetists. https://www.geoffreykayemuseum.org.au/the-great-women-of-anaesthesia-emily-hancock-siedeberg-mckinnon/.
Host, Emily O. 1990. “Emily H. Siedeberg-McKinnon.” In Women Doctors in New Zealand: An Historical Perspective, 1921-1986, 139-146. Auckland, New Zealand: ISMNZ.
Leichter, Jill. n.d. “Emily Siedeberg.” Jewish Online Museum. Accessed Feb 11, 2021. https://www.jewishonlinemuseum.net/emily-siedeberg.
Murray, David. 2016. “Emily Siedeberg’s House.” Built In Dunedin. https://builtindunedin.com/2016/07/25/emily-siedebergs-house/.
National Council Of Women of New Zealand. 1975. A New Earth: Pioneer Women of New Zealand. Wellington, New Zealand: National Council of Women of New Zealand.
Page, Dorothy. 2008. Anatomy of a Medical School: A History of Medicine at the University of Otago, 1875-2000. Dunedin, New Zealand: Otago University Press.
Parry, Gordon. 1975. Otago Medical School 1875-1975: An Historical Sketch. Dunedin, New Zealand: University of Otago.
Royal Society. n.d. “Emily Siedeberg.” Royal Society, Te Aparangi. Accessed Feb 11, 2021. https://www.royalsociety.org.nz/150th-anniversary/150-women-in-150-words/1867-1917/emily-siedeberg/.
Sargison, Patricia A. 1993. Notable Women in New Zealand Health = Te hauora ki Aotearoa : ōna wāhine rongonui. Auckland, New Zealand: Longman Paul.
Sargison, Patricia A. 1996. “Emily Hancock Siedeberg.” Te Ara – The Encyclopedia of New Zealand. https://teara.govt.nz/en/biographies/3s16/siedeberg-emily-hancock.
University of Otago. n.d. “Dr Emily Hancock Siedeberg Scholarship.” University of Otago Scholarships. Accessed Feb 11, 2021. https://www.otago.ac.nz/study/scholarships/database/otago014618.html.
Wanhalla, Angella. 2007. “To ‘Better the Breed of Men’: Women and Eugenics in New Zealand, 1900–1935.” Women’s History Review 16 (2): 163-182. 10.1080/09612020601048779.
Footnotes
[1] Sargison 1996; Creese and Creese 2010, p.146; Murray 2016; Sargison 1993, p.12.
[2] Murray 2016
[3] Cronin 2017; Leichter, n.d.; Murray 2016
[4] Host 1990, p.139; Sargison 1996.
[5] Host 1990, p.139.
[6] Creese and Creese 2010, p.146; Sargison 1996; Murray 2016; Sargison 1993, p.12.
[7] Murray 2016; Sargison 1993, p.13; Leichter, n.d.; Host 1990, p.139.
[8] Murray 2016.
[9] National Council Of Women of New Zealand 1975, p.62.
[10] National Council Of Women of New Zealand 1975, p.62.
[11] Host 1990, 139.
[12] National Council Of Women of New Zealand 1975, p.62; Host 1990, p.139
[13] Host 1990, p.139.
[14] Sargison 1996; Murray 2016.
[15] Sargison 1993, p.13; Host 1990, p.139.
[16] Belgrave 1988, p.46.
[17] Sargison 1993, p.12.
[18] Cronin 2017; Cronin 2018, p.9.
[19] Cronin 2017; Sargison 1993, p.13.
[20] Brookes 2017.
[21] Brookes 2017; National Council Of Women of New Zealand 1975, p.62; Cronin 2017; Host 1990, p.140.
[22] Host 1990, p.140.
[23] Sargison 1996; Page 2008, p.48.
[24] Host 1990, p.140.
[25] Leichter, n.d.; Sargison 1996.
[26] National Council Of Women of New Zealand 1975, p.63.
[27] Host 1990, p.140.
[28] Brookes 2017.
[29] Sargison 1996; Sargison 1993, p.13.
[30] Parry 1975, p.1.
[31] National Council Of Women of New Zealand 1975, p.63; Parry 1975, p.1; Sargison 1993, p.13.
[32] Sargison 1993, p.13.
[33] Brookes 2017.
[34] Leichter, n.d.; Murray 2016; Host 1990, p.139; National Council Of Women of New Zealand 1975, p.63; Page 2008, p.48.
[35] Sargison 1993, p.12.
[36] Leichter, n.d.; Host 1990, p.140; National Council Of Women of New Zealand 1975, p.63.
[37] Host 1990, p.140; Page 2008, p.48.
[38] Sargison 1993, pp.13-4; Brookes 2017.
[39] Creese and Creese 2010, p.146; Sargison 1996; Leichter, n.d.
[40] Royal Society, n.d.
[41] Belgrave 1988, p.51.
[42] Host 1990, 141.
[43] Murray 2016; Creese and Creese 2010, p.146; Royal Society, n.d.
[44] Brookes 2017; Murray 2016.
[45] Sargison 1996.
[46] Sargison 1993, p.14.
[47] Murray 2016; Sargison 1993, p.14.
[48] Sargison 1993, p.14.
[49] Host 1990, p.141.
[50] Host 1990, p.141.
[51] Sargison 1996; Creese and Creese 2010, p.147.
[52] Cronin 2017.
[53] Sargison 1993, p.14; Brookes 2017; Cronin 2018, p.9.
[54] Host 1990, pp.141, 143.; Leichter, n.d.
[55] Creese and Creese 2010, p.146.
[56] Sargison 1993, p.14.
[57] Creese and Creese 2010, p.147; Sargison 1996; Host 1990, p.141; Leichter, n.d.
[58] Cronin 2018, p.9.
[59] Host 1990, p.143; Cronin 2017.
[60] Cronin 2017; Cronin 2018, p.9.
[61] Host 1990, p.143.
[62] Cronin 2017.
[63] Leichter, n.d.; Brookes 2017.
[64] Host 1990, p.143
[65] Sargison 1993, p.14
[66] Cronin 2017; Sargison 1993, p.14; Host, p.143; Cronin 2018, p.9.
[67] Cronin 2017.
[68] Host 1990, p.143; Brookes 2017; Creese and Creese 2010, p.147.
[69] Sargison 1993, p.15.
[70] Brookes 2017; Cronin 2017.
[71] Cronin 2017.
[72] National Council Of Women of New Zealand 1975, p.62, Leichter, n.d.
[73] National Council Of Women of New Zealand 1975, p.62; Sargison 1993, p.15.
[74] Creese and Creese 2010, p.146; Cronin 2017; Sargison 1993, p.15.
[75] Host 1990, p.145.
[76] Sargison 1993, p.15
[77] Bryder 2014, p.15.
[78] Sargison 1993, p.15.
[79] Host 1990, p.145.
[80] Wanhalla 2007, p.170.
[81] Sargison 1996.
[82] Host 1990, p.144.
[83] Sargison 1993, p.15; Brookes 2017.
[84] Host 1990, p.144.
[85] Leichter, n.d.; Sargison 1993, p.15; Brookes 2017; Host 1990, p.144; Cronin 2018, p.9.
[86] Cronin 2017.
[87] Wanhalla 2007, p. 170; Sargison 1993, pp.14-15; Leichter, n.d.; Host 1990, p.144.
[88] Sargison 1993, p.15.
[89] Host 1990, p.144.
[90] Host 1990, pp.145-6.
[91] Host 1990, p.145; Leichter, n.d.
[92] Cronin 2017.
[93] Host 1990, p.141; Murray 2016; Sargison 1993, p.14.
[94] Murray 2016.
[95] Sargison 1996; Sargison 1993, p.15.
[96] Sargison 1993, p.15; Cronin 2017.
[97] Cronin 2017; Host 1990, p.143; Murray 2016.
[98] Sargison 1996; Murray 2016.
[99] Sargison 1993, p.15.
[100] Creese and Creese 2010, p.147.
[101] Murray 2016; Leichter, n.d.; Cronin 2017.
[102] Sargison 1996; Sargison 1993, p.15.
[103] University of Otago, n.d.
[104] Sargison 1996.
[105] Parry 1975, p.1.
